The Moment Medicine Realized It Was Only Reading the Headlines
For nearly a decade, clinical genetics revolved around a tidy, confident idea: if you can read the exome, you can explain the disease. It was elegant and logical. The exome represents the 1-2% of the genome that codes for proteins, and proteins run the body. So the exome must hold the answers or so we thought.
Whole Exome Sequencing (WES) entered medical practice like a superhero: fast, affordable, and data-rich. Hospitals embraced it. Families pinned their hopes on it. Clinicians felt, perhaps for the first time, that they had a genuine map to navigate rare diseases.
But then the unexpected happened.
Nearly half of all patients walked out with the same anticlimactic line in their report: “No pathogenic variant detected.” Not misdiagnosed -undiagnosed. Their symptoms were real, their family histories unmistakably genetic, but their exomes were whispering: “I can’t see the problem.”
It was the moment medicine realized it had been reading only the headlines of the human genome, while the real story was unfolding below -in the footnotes, the margins, the unexplored chapters no one had bothered to read.
In 2024, major studies from European and Asian genome programs confirmed this quietly growing suspicion: WES misses up to 50% of clinically relevant variants. And not because the diseases were mysterious -but because the exome was simply looking in the wrong place.
The Part of the Genome We Pretended Didn’t Matter
Science has a history of dismissing what it doesn’t understand. And for decades, the non-coding genome -a sprawling 98% of our DNA was labeled “junk.” It was one of the most damaging oversimplifications in modern biology.
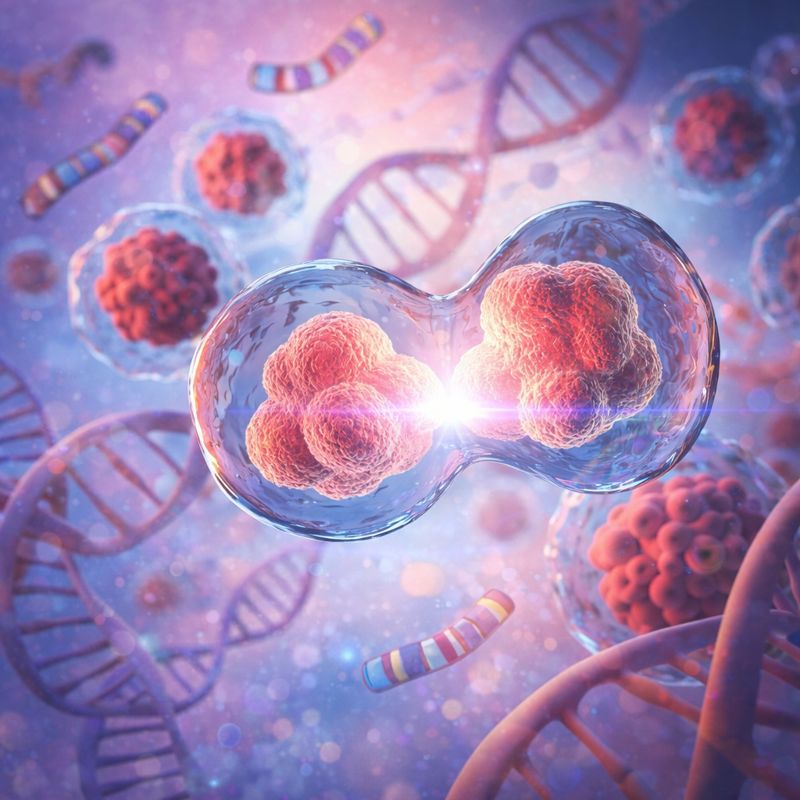
Because buried in that vast genomic terrain in deep introns, regulatory elements, enhancers, silencers, untranslated regions, and structural corridors were the keys to disorders we once believed were unsolvable.
By 2025, multiple studies had shown just how much lived in the places WES ignored:
- Deep intronic splice defects silently altering gene expression
- Regulatory variants flipping genes on and off like faulty electrical wiring
- Mitochondrial genome mutations driving metabolic and neuromuscular disease
- Structural rearrangements reshaping chromosomes without touching a single exon
- Repeat expansions -the genomic stutters behind Fragile X, myotonic dystrophy, and C9orf72-ALS -completely invisible to exome sequencing
The truth was uncomfortable but undeniable: the elegant 2% we knew wasn’t enough to explain the chaos in the 98% we ignored.
A 2025 Human Genetics and Genomics Advances report demonstrated that up to 20–25% of pathogenic variants lie entirely outside coding regions, while a Cell Reports Medicine long-read study revealed that many structural variants were systematically missed by WES for over a decade. Clinicians had been testing the wrong portion of the genome not out of neglect, but out of technological limitations.
Those limitations no longer exist.
Whole Genome Sequencing: When the Lights Finally Turned On
Whole Genome Sequencing (WGS) didn’t arrive quietly; it arrived like a floodlight.
Suddenly, the biology that had been hiding in the dark became impossible to ignore. Sequencing every base pair -not just the exons -revealed the full architecture of disease.
A child with unexplained seizures, originally labeled “inconclusive,” was revealed to have a deep intronic splice variant no exome had ever attempted to read. A family living with a mysterious three-generation neuromuscular disorder finally learned the cause -an inversion silently disrupting a critical gene.
A newborn in a neonatal ICU received a diagnosis within 72 hours through rapid WGS, altering clinical management before irreversible damage occurred.
And in cancer, the shift was seismic. Tumors once classified simply by organ “breast cancer,” “lung cancer,” “colon cancer” -began revealing mutational signatures, structural rearrangements, chromothripsis events, and genomic scars that predicted precisely which drugs would work and which would fail.
A 2025 Genetics in Medicine analysis demonstrated that:
- WGS identifies 43% more structural and splice-site variants vs. WES
- WGS achieves 33–45% diagnostic yield in first-line rare disease testing
- WGS delivers 20–30% additional diagnoses in exome-negative cases
And trio-based WGS (child + parents) has reached diagnostic rates as high as 57% in recent Asia-Pacific cohort studies.
Whole Genome Sequencing didn’t just find answers -it exposed how limited our vision had been all along.
We weren’t bad at diagnosing genetic disease. We were simply reading the wrong part of the genome.
The Human Cost of Looking in the Wrong Place
A missed diagnosis isn’t an academic inconvenience -it’s a human crisis.
It’s parents spending years bouncing between specialists. It’s invasive tests that never needed to happen. It’s the wrong medication. It’s a failed therapy. It’s surgeries done “just in case.” It’s financial strain disguised as resilience. It’s emotional exhaustion masquerading as patience.
It is families living inside a diagnostic fog when the answer was always there -just outside the narrow boundaries of the exome.
Whole Genome Sequencing changes that physics.
It collapses years into days. Confusion into clarity. Wandering into direction.
It gives clinicians a complete blueprint instead of a sketch. It gives families certainty instead of speculation. It gives patients something medicine often forgets to protect: the dignity of knowing the truth.
A 2024 global patient impact survey found that families receiving genome-first diagnostics reported three times greater emotional closure and significantly reduced medical expenditure, even when treatments were not available. Because a diagnosis is not just a label -it is a roadmap for care, prognosis, therapy selection, and informed reproductive decisions.
Genome sequencing, for many families, is not just a test. It is the end of suffering in the shadows.
Why India Cannot Afford to See Only 2% of Its Own Genome
India is not just another population in global genomics -India is a genomic universe. It is home to: unparalleled genetic diversity, deep-rooted patterns of endogamy, rare founder effects, the world’s largest pediatric population, 30–50 million rare disease patients Using exome-only approaches in a country like this is like mapping a megacity with a torch.
India needs the full illumination of the genome -its regulatory complexity, structural variation, mitochondrial architecture, and population-specific variants that are often absent in Western reference data.
In recent years, Indian clinical studies have shown that:
WGS captures region-specific disease variants that exomes routinely miss, Structural variants are significantly more common in certain Indian subpopulations, Mitochondrial disorders, often undetected by WES, are disproportionately represented For India, WGS is not a luxury -it is the only diagnostic strategy that matches the biological reality of 1.4 billion people. The future of Indian medicine will not be written in exons. It will be written in everything beyond them.
Closing Message: Medicine Moves Forward Only When It Stops Looking Away
For decades, we stared at two percent of our DNA and pretended we understood the whole human story.
We don’t get to do that anymore.
Whole Genome Sequencing doesn’t just offer more data- it offers the truth.
And the truth is this: The answers we’ve been searching for have always been there, written in the genome -in all of it, not just the parts we found convenient to read.
The future of medicine belongs to those willing to turn the final page.
“The genome isn’t the problem- our willingness to interpret it is. And the future will be built by those who stop hiding behind VUS and start reading the whole story.”
References:
- Ng HY, Ma W, Lam WJ, Lau CS, Luk HM, Au LWC, Cheng SSW, Chong JSC, Ho S, Ma BM, Pang SYY; Hong Kong Genome Project; Chu ATW, Chung BHY. Identification of technically challenging variants: Whole-genome sequencing improves diagnostic yield in patients with high clinical suspicion of rare diseases. HGG Adv. 2025 Jul 10;6(3):100469. doi: 10.1016/j.xhgg.2025.100469. Epub 2025 Jun 16. PMID: 40528347; PMCID: PMC12269974.
- Pandey R, Brennan NF, Trachana K, Katsandres S, Bodamer O, Belmont J, Veenstra DL, Peng S. A meta-analysis of diagnostic yield and clinical utility of genome and exome sequencing in pediatric rare and undiagnosed genetic diseases. Genet Med. 2025 Jun;27(6):101398. doi: 10.1016/j.gim.2025.101398. Epub 2025 Feb 25. PMID: 40022598.