Most of us visit a doctor only when we feel unwell. Traditional healthcare has largely been reactive—treating disease after symptoms appear. But genomics is helping change that approach. Today, genetic and genomic testing can sometimes identify health risks early, allowing people to take preventive steps before illness develops. This is called preventive or predictive genomics, and it is becoming an important part of modern healthcare.
To understand this, it helps to know the difference between predictive genetics and reactive testing. Reactive testing is done when someone already has symptoms or a diagnosis. For example, a person with cancer may undergo tumor testing to guide treatment, or a child with developmental delay may have genetic testing to find the cause. Predictive genetic testing is different. It is done when a person appears healthy, to identify inherited risks that may increase the chance of developing certain diseases in the future. The goal is not to predict the future with certainty, but to highlight risks that are high enough to justify earlier screening, closer monitoring, or preventive action.
One of the most well-known examples is hereditary cancer testing. Some people inherit gene changes that increase their risk of cancers such as breast, ovarian, colorectal, or prostate cancer. These risks may not be obvious from routine health checks. In some families, the same cancer appears in multiple relatives or occurs at younger ages. Genetic tests like hereditary cancer panels can identify these high-risk variants, allowing individuals to start screening earlier, undergo more frequent monitoring, or take preventive steps under medical guidance. This can mean finding cancer at an early, more treatable stage—or sometimes preventing it altogether.
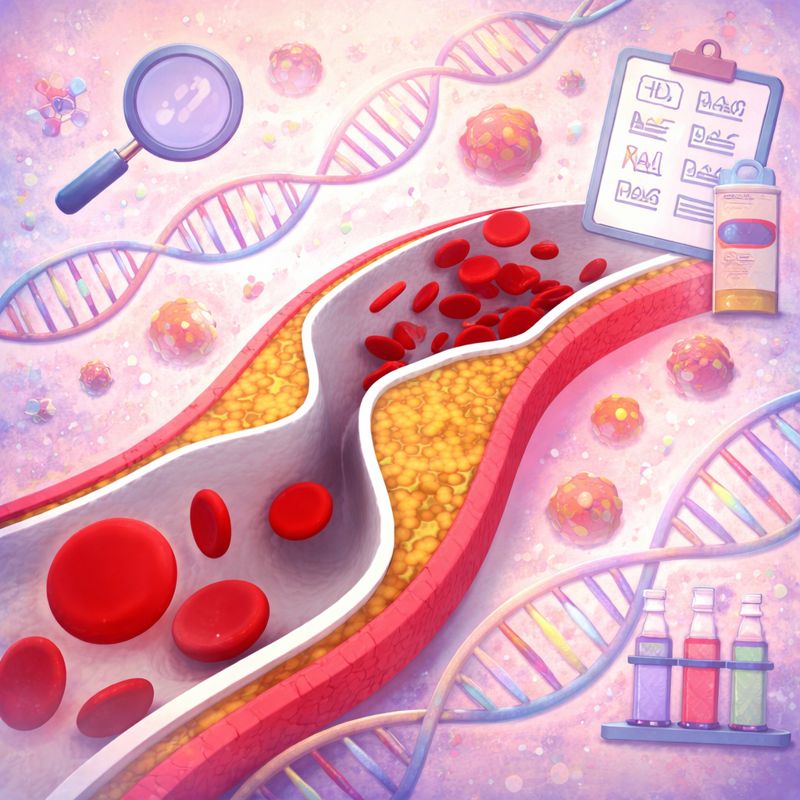
Another important area is cardiovascular genetics. Certain inherited variants can increase the risk of early heart disease, dangerously high cholesterol, or sudden heart rhythm problems. A person may look healthy on the outside, but still carry a genetic risk that could lead to a heart attack or sudden cardiac event at a young age. If identified early, preventive care becomes much more targeted. Doctors may recommend earlier cholesterol monitoring, lifestyle changes, regular heart evaluations, or medications that reduce risk long before a serious event happens.
Preventive genomics does not stop at identifying risk. What matters most is what you do next. A preventive plan may include earlier screening, such as starting colonoscopies or breast screening at a younger age than usual. It may involve more frequent follow-up visits, imaging, or blood tests. Lifestyle recommendations can also become more personalized—such as focusing on heart-protective habits if someone has inherited cardiovascular risk. In some cases, preventive medications or procedures may be considered, but only when the risk is clearly high and supported by clinical guidelines.
Whole Genome Sequencing (WGS) can take preventive testing further because it looks at nearly all of a person’s DNA in one test, rather than focusing on a small set of genes. This broader coverage can help detect rare but important inherited variants that targeted panels might miss. WGS also creates a long-term resource, because the same genomic data can be reinterpreted in the future as science advances, potentially revealing new insights over time.
So when should someone consider predictive genetic testing? It is especially worth discussing if you have a strong family history of cancer, heart disease at a young age, sudden unexplained deaths, or rare inherited disorders. It can also be valuable for people planning a pregnancy, particularly in communities where consanguinity or endogamy is common, as this can increase the chance of shared recessive genetic risks. Even without a clear family history, some individuals choose preventive testing because they want a deeper understanding of their health risks and a more proactive approach to long-term wellbeing.
In summary, genomics cannot predict every disease, and it cannot replace healthy habits or regular medical care. But it can identify certain high-impact inherited risks early, when prevention and screening can make the biggest difference. As preventive healthcare becomes a growing priority, predictive genomics—and especially comprehensive approaches like Whole Genome Sequencing —offers an actionable, forward-looking way to stay healthier for longer.